“Crisis and deadlocks when they occur have at least this advantage, they force us to think.” Jawaharlal Nehru
- The unattractiveness of the programs. They involve extensive coursework and when the returns come in, it takes several years and a lot o good luck for one to live comfortably unlike in some professions. Predominantly true for nurses.
- Immigration to better-paying continents. In the past four years, one can account for at least four health workers who have relocated abroad.
- The ambiguity of our roles in our home countries. The scope of practice within our set up is limited and a lot of medical hegemony preexists.
- Lack of provision of our basic items. Anyone working in the public healthcare systems in most African countries such as Kenya always complains of inadequate resources such as personal protective gear and hospital utilities.
- Health workers are among the groups that face the greatest numbers of levels of burn out. To obtain more information on the above you may follow the link below. https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-019-7566-7
1.To our leaders
- Use it as a future reference point in advocating for increased allocation of monetary funds towards emergencies, healthcare, water and sanitation, and special needs groups. This would help cushion our economies in times such as this when we will soon be facing a global recession.
- Have more healthcare workers who are actively participating in decision-making levels. I have to insist they should be people who have extensively worked within the clinical set up then transitioned to leadership and management. Most of our current policies and strategies do not work because there is a disconnect among those who generate them and those who should apply them.
- Stop being greedy. It is unfortunate we are bearing the brunt for misappropriated funds. Pandemics offer a great lesson on self-reflection because with our poorly managed health systems and a global crisis there is nowhere for even the leaders to run and hide. The same issues facing the public hospitals will soon be facing the private healthcare.
- Collaborative interactions in different sectors.
2.To all health workers
- Curb medical hegemony. The nature of functional working relationships in healthcare is often a point of concern. With supremacy battles, day in day out we tend to forget the core of our call which is health maintenance, health promotion, and disease prevention. This then leads to the medicalization of every intervention whilst at times all we need to do is educate our patients on practices as simple as, adopting basic hand hygiene, better waste disposal, and safe food preparation. We have forgotten that improved economic power does not directly correlate with these practices.
- Work strategically to enhance ourselves to be in positions where we can at least try to implement and effect appropriate change. The moment we take a back seat on issues that directly affect healthcare then we place ourselves at risk. For instance, during this current pandemic, On the 11th of March Italy, among the hardest-hit regions globally had approximately 2,629 infected health care workers and with their very high death rates, we can only assume that it is just as high among the infected health workers. Now translate that to Africa.
- Re-evaluate our curriculums. Do we feel very prepared by the end of our academic journey? During pandemics it offers an opportunity to assess our proficiency, efficiency, and innovativeness. What can we do with what we have while trying to save as many lives as possible? Are we capable of it? Some suggestions would be the provision of telehealth this maybe consultation, counseling services, etc.
- Seek counseling, during and after the crisis. It is already very overwhelming. It may actually get way worse before it gets better. We need an outlet for all we are currently feeling if we are to be effective at our jobs.
3. To all of us
In all pandemics basic principles that always work are;
- Learn how it is being spread and put measures to mitigate that as per the causative agent.
- Always keep a travel diary noting areas visited. Record your health status pre and post.
- Work towards improving your immunity and health status. It may not prevent you from getting ill but it provides a better opportunity on surviving.
- Practice saving no matter how little it comes in handy when one needs to make emergency purchases
- Always adhere to the basic principles of hand hygiene, cough etiquette, proper waste disposal, and food safety.
- Be humane, not everyone has the economic power to purchase in bulk so do not forget to help those in need at such times.
To read more on previous pandemics please follow the links below
In conclusion, as we try to overcome this current threat lets ponder on one of the many great quotes by Aristotle.
"A smooth sea never made a skillful sailor; we learn greatly from the storms in our lives and what we already know finally comes in useful."

 "How we care for the dying is an indicator of how we care for all sick and vulnerable people. It is a measure of society as a whole and it is a litmus test for health and social care services"(DOH 2008).
"How we care for the dying is an indicator of how we care for all sick and vulnerable people. It is a measure of society as a whole and it is a litmus test for health and social care services"(DOH 2008).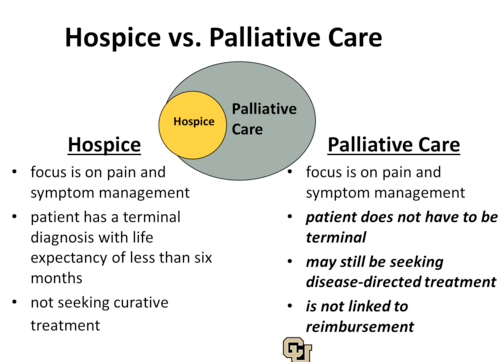 We often assume that it is such a foreign concept in our African set up yet we have been applying it unknowingly for many years. For instance how often do we allow for the religious leaders to pray for the very sick in our workstations? Palliative care should begin at diagnosis, it involves a multidisciplinary approach that is directed to the patient and family. It is distinguished from hospice care in that hospice care involves providing care for a person with a terminal illness whom doctors believe he or she has 6 months or less to live if the illness runs its natural course. Attempts to cure the illness are terminated in hospice care. The main goals here are to relieve pain while promoting comfort physically and psychologically.
We often assume that it is such a foreign concept in our African set up yet we have been applying it unknowingly for many years. For instance how often do we allow for the religious leaders to pray for the very sick in our workstations? Palliative care should begin at diagnosis, it involves a multidisciplinary approach that is directed to the patient and family. It is distinguished from hospice care in that hospice care involves providing care for a person with a terminal illness whom doctors believe he or she has 6 months or less to live if the illness runs its natural course. Attempts to cure the illness are terminated in hospice care. The main goals here are to relieve pain while promoting comfort physically and psychologically. Advance care directives refer to a formal representation of the discussed health care goals. They are necessary for they help communicate one's desires in the event one becomes incapable of consenting to or refusing treatment or other care. In the generation of these goals, the following ethical principles should be maintained
Advance care directives refer to a formal representation of the discussed health care goals. They are necessary for they help communicate one's desires in the event one becomes incapable of consenting to or refusing treatment or other care. In the generation of these goals, the following ethical principles should be maintained