 "How we care for the dying is an indicator of how we care for all sick and vulnerable people. It is a measure of society as a whole and it is a litmus test for health and social care services"(DOH 2008).
"How we care for the dying is an indicator of how we care for all sick and vulnerable people. It is a measure of society as a whole and it is a litmus test for health and social care services"(DOH 2008).For adults it ;
- provides relief from pain and other distressing symptoms;
- affirms life and regards dying as a normal process;
- intends neither to hasten or postpone death;
- integrates the psychological and spiritual aspects of patient care;
- offers a support system to help patients live as actively as possible until death;
- offers a support system to help the family cope during the patients' illness and in their own bereavement;
- uses a team approach to address the needs of patients and their families, including bereavement counseling, if indicated;
- will enhance the quality of life, and may also positively influence the course of illness;
- is applicable early in the course of illness, in conjunction with other therapies that are intended to prolong life, such as chemotherapy or radiation therapy, and includes those investigations needed to better understand and manage distressing clinical complications.
For the pediatric definition of the same please follow the link https://www.who.int/cancer/palliative/definition/en/.
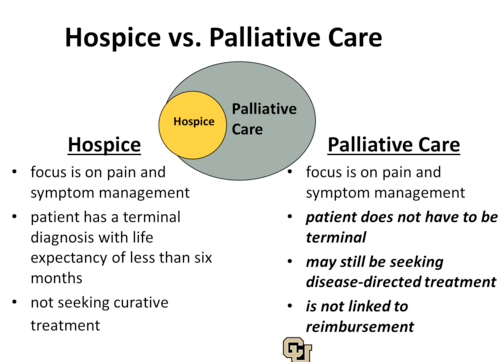 We often assume that it is such a foreign concept in our African set up yet we have been applying it unknowingly for many years. For instance how often do we allow for the religious leaders to pray for the very sick in our workstations? Palliative care should begin at diagnosis, it involves a multidisciplinary approach that is directed to the patient and family. It is distinguished from hospice care in that hospice care involves providing care for a person with a terminal illness whom doctors believe he or she has 6 months or less to live if the illness runs its natural course. Attempts to cure the illness are terminated in hospice care. The main goals here are to relieve pain while promoting comfort physically and psychologically.
We often assume that it is such a foreign concept in our African set up yet we have been applying it unknowingly for many years. For instance how often do we allow for the religious leaders to pray for the very sick in our workstations? Palliative care should begin at diagnosis, it involves a multidisciplinary approach that is directed to the patient and family. It is distinguished from hospice care in that hospice care involves providing care for a person with a terminal illness whom doctors believe he or she has 6 months or less to live if the illness runs its natural course. Attempts to cure the illness are terminated in hospice care. The main goals here are to relieve pain while promoting comfort physically and psychologically.- It improves patient care outcomes by directing focus on care and not problem-solving.
- It increases patient and family satisfaction by generating increased value of patients' preferences and opinions.
- It is cost-saving to the patient, family, and institutions through the reduction of unnecessary interventions at the end of life, it reduces insurance premiums and reduces the practice of defensive medicine.
Follow the link for more information on this https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5360382/.
 Advance care directives refer to a formal representation of the discussed health care goals. They are necessary for they help communicate one's desires in the event one becomes incapable of consenting to or refusing treatment or other care. In the generation of these goals, the following ethical principles should be maintained
Advance care directives refer to a formal representation of the discussed health care goals. They are necessary for they help communicate one's desires in the event one becomes incapable of consenting to or refusing treatment or other care. In the generation of these goals, the following ethical principles should be maintained- Autonomy – people have the right to control what happens to their bodies.
- Beneficence – do the most good for the patient in every situation.
- Nonmaleficence – first “do no harm” is the bedrock of medical ethics, in every situation.
- Justice – try to be as fair as possible when offering treatment to patients and allocating scarce medical resources.
Benefits of ACD include;
- Ensures self-determination and an increase in quality of life near the end of life.
- Research shows it decreases emotional conflict.
- When patients’ desires are met, patients, their loved ones and clinicians have peace of mind.
- There is reduced stress, anxiety and depression for surviving relatives and advocates.
- Advance directives and advance care planning facilitate communication.
Please follow the link for more information http://kehpca.org/advance-care-planning-in-kenya-starting-the-conversation/.
Barriers to implementing goal-directed care include
Barriers to implementing goal-directed care include
- General practitioners characteristics
- Perceived patient characteristics -Some studies show that patients with a more defined disease course are more likely to vouch for goal-directed healthcare.
- Health care system characteristics -Is it problem-based or patient-centered.
- Lack of skills to deal if one is not enlightened in this they will not be in a position to initiate the conversation.
- Vague requests -
- Difficulties with defining the right moment -This is primarily true for health conditions that have an acute onset and have a poor prognosis.
- The attitude that patients should initiate ACP
- Fear of depriving them of hope- For some people, the discussion of death still alludes to "wishing of sudden death".
For continued enlightenment in these topics please follow the links below;
https://onlinelibrary.wiley.com/doi/full/10.1111/scs.12315
https://www.tandfonline.com/doi/full/10.3109/02813432.2013.854590
https://www.tandfonline.com/doi/full/10.3109/02813432.2013.854590
As we aim to create a more humane health system we should seek to remember that
👌👌
ReplyDelete